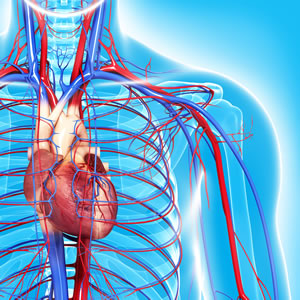
Inflammation and irritation of the coronary (heart) artery inner lining can be caused by years of smoking and uncontrolled hypertension and diabetes. These inflamed areas can start to collect cholesterol from the blood stream and begin to form plaque. This plaque begins to grow and decreases the diameter of the artery which compromises blood flow. This decrease can then potentially cause angina (chest pain) symptoms.
In certain situations, this plaque in the artery may rupture or break open which can lead to a formation of a clot in the coronary artery. The clot can block part of the artery preventing the oxygen-rich blood from being delivered to the heart muscle. Part of the heart can then die.
This is known as a heart attack or myocardial infarction. If action is not taken immediately and the condition treated, the part of the heart muscle not receiving oxygen may not be revived and is replaced with scar tissue. Over time, this scar tissue may hinder the ability of the heart to pump effectively and can lead to ischemic (lack of oxygen) cardiomyopathy. It can also lead to electrical conduction irregularities causing abnormal heart rhythms such as ventricular tachycardia or ventricular fibrillation which are associated with sudden cardiac death.
The 4 Steps of Atherosclerosis Development
Step 1:
Injury to inner cell lining
Inside of the artery consists of a single layer of cells called the endothelium, which protects the other layers from interacting with blood. Agents such as smoking, hypertension, elevated LDL levels and stress can potentially cause injury to the endothelium causing atherosclerotic
Step 2:
Relocation of inflammatory cells
When atherosclerotic lesions develop, the endothelial cells (inner layer of cells) cells start to bind to monocytes and other inflammatory cells that start atherosclerotic lesions. Once in these lesions, the monocytes start to travel between the inner lining of the artery and localize in the next layer (intima) where they transform into macrophages and start to engulf mainly LDL.
Step 3:
Accumulation and Smooth Muscle Cell Production
Smooth muscle cells move into the intima and divide. The macrophages that digest the lipids ultimately transform into foam cells that is protective in that it removes excess lipids from circulation. However, this accumulation eventually leads to the progress of the lesion. Active macrophages tarnish (oxidize) LDL and digest them to become foam cells. Macrophages and smooth muscle cells release collagen and other proteins.
Step 4:
Plaque structure
The plaque is now mature and is a collection of foam cells, proteins, smooth muscle cells, and cholesterol debris. This plaque can then harden, crack, cause blood clots to form, and even occlude (block) the vessel.
The information for this course is taken from the FLS continuing education course “Healthy Heart for a Healthy Life” by Tina Schmidt-McNulty.
For more information about working with clients with chronic disease, see the Fitness Learning Systems Chronic Disease and Exercise Specialist Certificate Program. Specialize and become recognized as a medical fitness professional. Fitness Learning Systems is an IACET accredited continuing education provider.


